Depression is a pervasive and intricate mental health condition that transcends mere feelings of sadness; it permeates the very fabric of one’s being, reshaping perceptions, thoughts, and actions. Yet, despite its prevalence and impact on millions worldwide, depression remains a misunderstood and stigmatized phenomenon. In this article, we embark on a journey to unravel the complexities of depression, aiming to shed light on its multifaceted nature and provide insights into its causes, symptoms, and treatment options.
Imagine waking up each day with a heavy weight pressing down on your chest, suffocating your spirit, and draining the color of the world around you. This is the reality for those grappling with depression—a relentless battle against invisible demons that assail the mind and soul.
Contrary to common misconceptions, depression is not a fleeting amount of sadness that can be brushed aside with a simple smile or cheerful distraction. It is a profound and enduring state of despair, characterized by profound sadness, apathy, and an overwhelming sense of hopelessness.
What sets depression apart from occasional feelings of melancholy is its persistence and pervasiveness. It lingers like a shadow, casting a pall over every aspect of life—from relationships and work to physical health and self-perception. It robs individuals of their vitality, and their zest for life, leaving them adrift in a sea of numbness and despair. Yet, amidst the darkness, there is a glimmer of hope—a recognition that understanding depression is the first step towards healing and reclaiming one’s sense of self.

What is Depression?
Depression, clinically known as major depressive disorder (MDD), is a serious mental illness characterized by persistent feelings of sadness, hopelessness, and a loss of interest in activities once enjoyed. It affects how individuals think, feel, and handle daily activities, often leading to significant impairment in social, occupational, and other important areas of functioning. Look at this site if you want to understand depression via video and animation.
Types of Depression:
Depression manifests in various forms, including:
1. Major Depressive Disorder (MDD):
The most common form of depression is characterized by persistent low mood and loss of interest in activities.
2. Persistent Depressive Disorder (PDD):
Formerly known as dysthymia, this type involves long-term but less severe symptoms of depression.
3. Bipolar Disorder:
Features periods of depression alternating with episodes of mania or hypomania.
4. Seasonal Affective Disorder (SAD):
Occurs seasonally, typically in the winter months, due to reduced exposure to sunlight.
5. Postpartum Depression:
Affects new mothers after childbirth, characterized by mood swings, anxiety, and exhaustion.
Causes of Depression:
Understanding depression requires a nuanced exploration of its multifaceted causes, which encompass a complex interplay of biological, psychological, social, and environmental factors. While it’s essential to recognize that depression can manifest differently in each individual, several common underlying contributors contribute to its onset and persistence:
1. Genetic Predisposition
Genetics plays a significant role in predisposing individuals to depression. Research indicates that individuals with a family history of depression are at a higher risk of developing the condition themselves. Specific genetic variations may influence neurotransmitter function, brain structure, and stress response, contributing to susceptibility.
2. Neurochemical Imbalance
Depression is closely linked to imbalances in neurotransmitters—chemical messengers that regulate mood, emotions, and cognition. Low levels of serotonin, dopamine, and norepinephrine have been implicated in depressive symptoms. These imbalances may arise from genetic factors, environmental stressors, or disruptions in neural pathways.
3. Brain Structure and Function
Neuroimaging studies have revealed structural and functional abnormalities in the brains of individuals with depression. Areas involved in mood regulation, such as the prefrontal cortex, hippocampus, and amygdala, may exhibit alterations in volume, connectivity, or activity. These changes can impact emotional processing, memory, and stress response, contributing to depressive symptoms.
4. Psychological Factors
Psychological vulnerabilities, such as negative cognitive patterns, low self-esteem, and maladaptive coping strategies, can predispose individuals to depression. Chronic stress, trauma, or unresolved emotional conflicts may exacerbate these vulnerabilities, leading to the onset or exacerbation of depressive symptoms. Additionally, personality traits like perfectionism or neuroticism may increase susceptibility to depression.
5. Life Events and Stressors
Adverse life events, such as the loss of a loved one, relationship difficulties, financial problems, or work-related stress, can trigger or precipitate depression. These stressors disrupt one’s sense of stability and security, overwhelming coping mechanisms and precipitating a cascade of negative emotions. The cumulative burden of chronic stressors may also contribute to the development of depression over time.
6. Chronic Illness and Medical Conditions
Certain medical conditions, such as chronic pain, autoimmune disorders, neurological diseases, and hormonal imbalances, are associated with an increased risk of depression. The burden of managing these conditions, coupled with the physical symptoms they entail, can contribute to emotional distress and exacerbate depressive symptoms. Furthermore, medications used to treat these conditions may have side effects that impact mood and cognition.
7. Substance Abuse
Substance abuse and dependence frequently co-occur with depression, creating a complex interplay of causes and consequences. Individuals may turn to alcohol, drugs, or other substances as a maladaptive coping mechanism to numb emotional pain or alleviate distress. However, substance abuse can exacerbate underlying depression, impair judgment, and interfere with treatment outcomes.
8. Social and Environmental Factors:
Socioeconomic disparities, social isolation, discrimination, and lack of social support can significantly impact mental health and contribute to the development of depression. Living in environments characterized by poverty, violence, or instability increases exposure to chronic stressors and reduces access to resources and opportunities for recovery. Additionally, cultural norms and societal attitudes towards mental illness may influence help-seeking behaviors and contribute to stigma.
It’s important to recognize that depression is not solely determined by any single factor but arises from the complex interplay of multiple influences. By addressing these underlying causes holistically and adopting a biopsychosocial approach to treatment, individuals can receive comprehensive care tailored to their unique needs. Moreover, fostering awareness, resilience, and social support can mitigate risk factors and promote mental well-being across diverse populations.
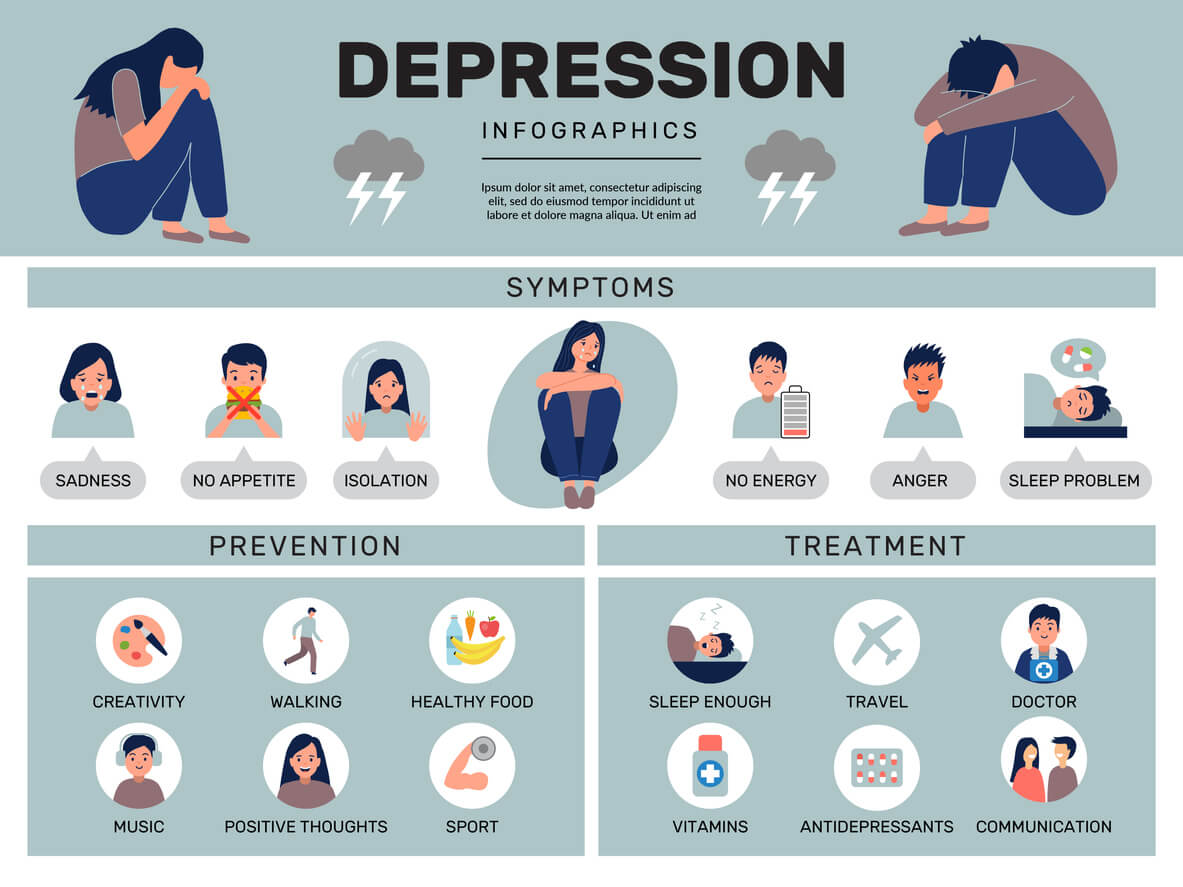
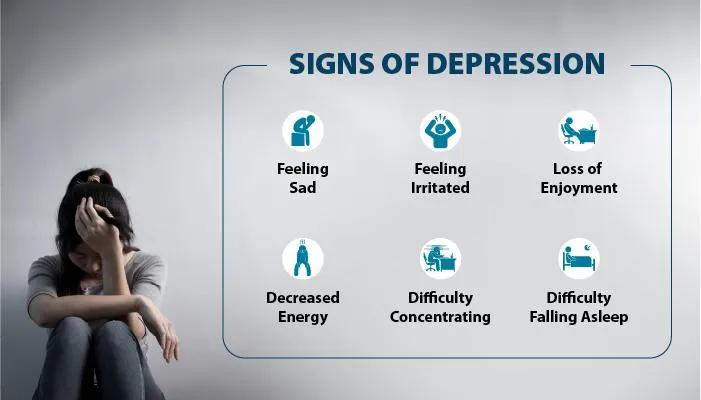
Symptoms of Depression:
Recognizing the symptoms of depression is crucial for early intervention and treatment. Common signs include:
1. Persistent sadness, emptiness, or hopelessness
2. Loss of interest in previously enjoyed activities
3. Changes in appetite or weight
4. Sleep disturbances, either insomnia or excessive sleeping
5. Fatigue or loss of energy
6. Feelings of worthlessness or excessive guilt
7. Difficulty concentrating or making decisions
8. Thoughts of death or suicide
It’s essential to note that not everyone with depression experiences all these symptoms, and their severity can vary from person to person.
Effects of Depression:
Depression extends beyond emotional distress and can significantly impact various aspects of an individual’s life:
1. Relationships:
Strained relationships due to withdrawal, irritability, or emotional numbness.
2. Work or School:
Reduced productivity, absenteeism, or difficulty concentrating.
3. Physical Health:
Increased risk of chronic illnesses like heart disease, diabetes, and chronic pain.
4. Substance Abuse:
Some individuals turn to alcohol or drugs as a way to cope with depressive symptoms, leading to substance abuse disorders.
5. Suicidal Thoughts:
Severe depression can culminate in suicidal ideation or suicide attempts, necessitating immediate intervention.
Treatment Options:
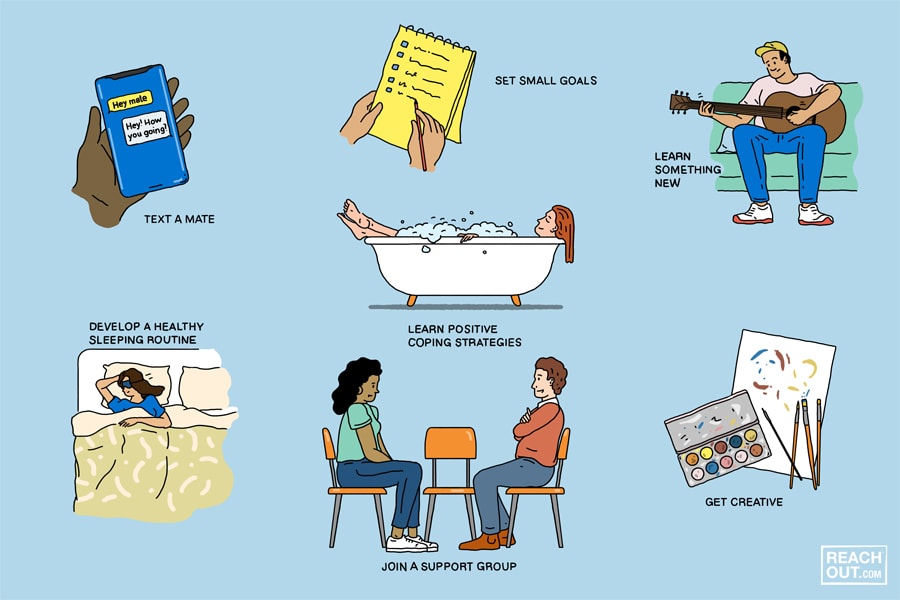
Managing depression involves a multifaceted approach that integrates pharmacological interventions, psychotherapy, lifestyle modifications, and support systems. Tailoring treatment to individual needs and preferences is essential for optimizing outcomes and promoting long-term recovery. Here, we explore various treatment options available for depression:
Psychotherapy:
Cognitive-Behavioral Therapy (CBT):
CBT is a widely researched and effective form of psychotherapy for depression. It focuses on identifying and challenging negative thought patterns and replacing them with more adaptive beliefs and behaviors. CBT equips individuals with practical skills to cope with stress, manage symptoms, and prevent relapse.
Interpersonal Therapy (IPT):
IPT addresses interpersonal conflicts and relationship issues that contribute to depression. It aims to improve communication skills, resolve conflicts, and enhance social support networks. By exploring patterns of interaction and addressing underlying relational dynamics, IPT helps individuals develop healthier relationships and improve mood.
Mindfulness-Based Therapy:
Mindfulness-based approaches, such as mindfulness-based cognitive therapy (MBCT) and mindfulness-based stress reduction (MBSR), integrate mindfulness practices with cognitive and behavioral techniques. These approaches cultivate present-moment awareness, acceptance, and self-compassion, reducing rumination and promoting emotional regulation.
Medication:
Antidepressants:
Antidepressant medications, including selective serotonin reuptake inhibitors (SSRIs), serotonin-norepinephrine reuptake inhibitors (SNRIs), tricyclic antidepressants (TCAs), and others, are commonly prescribed to alleviate depressive symptoms. These medications work by modulating neurotransmitter levels in the brain, improving mood, and reducing symptoms of depression. It’s essential to work closely with a healthcare provider to find the most effective medication and dosage with minimal side effects.
Augmentation and Combination Therapy:
In cases of treatment-resistant depression or severe symptoms, healthcare providers may recommend augmenting antidepressant therapy with other medications, such as atypical antipsychotics or mood stabilizers. Additionally, combining medication with psychotherapy can enhance treatment outcomes by addressing both biological and psychological aspects of depression.
Lifestyle Modifications:
Regular Exercise:
Engaging in regular physical activity, such as aerobic exercise, strength training, or yoga, can have significant benefits for mood and overall well-being. Exercise releases endorphins, reduces stress hormones, and improves sleep quality, which can alleviate depressive symptoms.
Healthy Diet:
Adopting a balanced diet rich in fruits, vegetables, whole grains, lean proteins, and omega-3 fatty acids supports brain health and mood regulation. Limiting the consumption of processed foods, sugary snacks, and caffeine may also help stabilize mood and energy levels.
Sleep Hygiene:
Prioritizing adequate sleep and practicing good sleep hygiene habits, such as maintaining a consistent sleep schedule, creating a relaxing bedtime routine, and minimizing screen time before bed, can improve sleep quality and alleviate symptoms of depression.
Supportive Interventions:
Support Groups:
Participating in mental health support groups or peer-led programs provides opportunities for individuals with depression to connect with others who share similar experiences, gain validation and empathy, and learn coping strategies.
Family Therapy:
Involving family members in therapy can enhance communication, address family dynamics, and strengthen support networks. Family therapy helps improve understanding, empathy, and collaboration in managing depression within the family system.
Complementary and Alternative Therapies:
Acupuncture:
Acupuncture, a traditional Chinese medicine practice involving the insertion of thin needles into specific points on the body, may help alleviate depressive symptoms by modulating neurotransmitter levels and reducing stress.
Herbal Supplements:
Some individuals may explore the use of herbal supplements or botanical remedies, such as St. John’s wort, omega-3 fatty acids, or S-adenosylmethionine (SAMe), as adjunctive treatments for depression. However, it’s essential to consult with a healthcare provider before using these supplements, as they may interact with medications or have side effects.
Electroconvulsive Therapy (ECT) and Transcranial Magnetic Stimulation (TMS):
ECT:
Electroconvulsive therapy is a medical procedure that involves the administration of controlled electrical currents to the brain to induce a seizure. ECT is typically reserved for severe, treatment-resistant depression or when rapid symptom relief is needed. It is often considered when other treatments have been ineffective or poorly tolerated.
TMS:
Transcranial magnetic stimulation is a non-invasive procedure that uses magnetic fields to stimulate nerve cells in the brain. TMS is FDA-approved for the treatment of depression and may be considered as an alternative or adjunctive therapy for individuals who have not responded to antidepressant medications.
Individuals with depression need to work closely with a healthcare provider to develop a comprehensive treatment plan tailored to their unique needs and preferences. Treatment may involve a combination of different modalities, and adjustments may be made based on response to therapy and changes in symptoms over time.
Additionally, maintaining open communication with healthcare providers, adhering to treatment recommendations, and engaging in self-care practices are essential components of long-term management and recovery from depression.
Conclusion:
Understanding depression goes beyond acknowledging its surface-level symptoms; it requires delving into its intricate layers of causative factors, manifestations, and treatment modalities. By fostering awareness, empathy, and access to effective interventions, we can collectively combat the stigma surrounding depression and pave the way for holistic healing and recovery. Remember, reaching out for help is not a sign of weakness but a courageous step toward reclaiming one’s mental health and well-being.
As we embark on this journey, let us remember that depression does not discriminate—it affects people of all ages, genders, and backgrounds. It is a universal human experience, one that transcends cultural boundaries and societal norms. By coming together to shine a light on depression, we can create a brighter, more compassionate world where everyone has the opportunity to thrive.